What's the Cheapest Medical Billing Service in 2025?
We understand that no one wants a “cheap” medical billing service—but when it's time to pay the bill, everyone wants the most affordable option without sacrificing quality. In this article, we’ll explore some of the most cost-effective medical billing companies, highlight key factors to consider when choosing a provider, and share best practices to help you get the best value for your money.
Here are 5 of the cheapest medical billing service companies offering affordable solutions for small practices and independent healthcare providers. Each listing includes a brief description and their most recently known pricing (as of 2024–2025):
1. Kareo
Description: Kareo is a popular cloud-based platform designed for small practices. It offers integrated billing, EHR, and practice management tools. It’s ideal for independent providers who want an all-in-one solution at an affordable cost.
-
Known Pricing: Starts at $125 per provider/month (for billing module only)
-
Notable Features: Real-time claim tracking, analytics, and compatibility with 3rd-party clearinghouses.
2. DrChrono
Description: DrChrono is an EHR and medical billing platform known for its scalability and customizable workflows. It’s widely used by small to mid-sized practices and offers flexible billing services through partners.
-
Known Pricing: Starts at 6% of monthly collections or custom quote depending on specialty and volume
-
Notable Features: Integrated EHR, appointment scheduling, e-prescribing, and patient portal.
3. PracticeSuite
Description: PracticeSuite is a budget-friendly medical billing and practice management solution. It supports both in-house and outsourced billing and is designed for growing practices.
-
Known Pricing: Free plan available (limited features); Paid billing packages start around $99/month per user
-
Notable Features: Denial management, insurance eligibility checks, and customizable reporting.
4. AdvancedMD
Description: AdvancedMD provides full RCM (revenue cycle management) and medical billing services tailored to both large and small healthcare organizations. It offers flexible pricing models based on collections or a flat fee.
-
Known Pricing: Starts at 4%–8% of monthly collections
-
Notable Features: Claims scrubbing, EHR integration, telemedicine, and extensive reporting tools.
5. MBMS (Medical Billing and Management Services)
Description: MBMS is a full-service medical billing company focusing on radiology, pathology, and other specialties. It’s known for its affordable rates and personalized service.
-
Known Pricing: Typically 4%–6% of monthly collections
-
Notable Features: Customizable billing strategies, payer analytics, and U.S.-based support.
💡 Quick Comparison Table:
| Company | Starting Price | Best For | Model Type |
|---|---|---|---|
| Kareo | $125/month/provider | Small practices | Flat monthly fee |
| DrChrono | ~6% of monthly collections | Growing clinics | % of collections |
| PracticeSuite | $99/month/user | Startups & budget-focused | Flat or hybrid |
| AdvancedMD | 4%–8% of collections | Midsize to large practices | % of collections |
| MBMS | 4%–6% of collections | Specialty groups | % of collections |
Healthcare providers choose a medical billing service is an important choice for any healthcare provider, affecting both financial health and patient satisfaction.
While the allure of budget-friendly options is tempting, it comes with a caveat. This article highlights the potential pitfalls of choosing the cheapest medical billing services, including limited offerings, hidden fees, inexperienced staff, and compliance issues.
By acknowledging these challenges, you will make a wise choice that prioritizes quality and accuracy over cost alone.
Read on to discover key considerations and best practices for selecting the right service for your needs.
1. Limited Services Offered in Medical Billing
Some billing companies offer limited services, which greatly reduces healthcare providers' ability to maximize their revenue management. This often leads to frustration among those looking for affordable billing solutions and healthcare billing practices that meet their specific needs. Knowing about each service option is important for making informed decisions, especially when you think about cost and quality in medical billing.
To provide a smooth billing experience, a trustworthy medical billing company should offer key services and billing efficiency. These include:
- Thorough handling of insurance claims and claims denial management
- Accurate medical coding and coding services
- Effective patient billing systems and medical accounts receivable
These components are critical, as they directly influence the accuracy and speed of reimbursements. Specialized services designed for different healthcare areas, like mental health, immediate medical attention, and surgery, can increase earning potential.
By addressing the distinct challenges that different specialties face and utilizing billing specialists, healthcare providers achieve better financial outcomes and focus more on patient care instead of financial complications

2. Potential for Hidden Fees
When potential clients select the cheapest medical billing service, they must remain wary of hidden fees in electronic billing that can accumulate unexpectedly, ultimately undermining the promise of affordable medical billing solutions. Transparency in pricing and clear communication regarding service costs are essential for maintaining trust and ensuring accurate financial forecasting.
Many providers include setup fees, surprising those initially attracted by a low monthly rate. Transaction fees tied to each claim submitted or received can quickly add up, impacting the overall savings.
Clients should also be aware of charges for extra services in billing operations that are not always made clear upfront, like reporting or support enhancements.
Creating a transparent atmosphere regarding costs and fees improves client satisfaction and the smooth running of operations for billing services, enabling healthcare providers to make decisions based on thorough financial information.
3. Lack of Personalized Support
Many healthcare providers find that not having customized support from medical billing outsourcing companies and healthcare finance professionals leads to inefficiencies and lower client satisfaction, which ultimately affects their practice's profitability. Clear communication and committed customer support are important for handling specific billing issues and solving problems before they arise.
Personalized help is important in billing because it lets billing specialists and medical billing consultants learn more about each practice and what they need.
Building strong connections with healthcare providers allows these specialists to provide customized solutions that directly tackle usual issues like coding mistakes and claim rejections.
Working closely together makes medical invoice processing and claims tracking more accurate and faster. It also makes it easier to collect payments from patients, increasing satisfaction for both healthcare providers and patients.
Ultimately, when providers receive attentive and customized billing support, they improve the overall financial health of their practice, allowing them to focus more on patient care.
4. Inexperienced Staff
Inexperienced staff within billing companies cause detrimental errors in billing accuracy standards in billing accuracy, negatively affecting healthcare reimbursement, medical claims processing, and increasing claim denials. Healthcare providers should work with billing companies that have experienced billing professionals who know medical coding and insurance verification to improve their revenue cycle management.
Healthcare providers benefit greatly when they work together with experienced billing staff to make sure claims are processed correctly the first time.
With proper training and practical experience, these professionals confidently handle the complicated details of insurance policies and requirements. This knowledge reduces mistakes and smooths and speeds up the claims process with automated billing.
Experienced staff often spot potential problems early, allowing them to implement quick fixes that protect the provider's income. Such proactive approaches improve cash flow and overall satisfaction for both healthcare providers and the patients they serve.
5. Potential for Errors and Inaccuracies
Errors and inaccuracies in healthcare billing can lead to serious repercussions, including denied claims and delayed reimbursements that hinder a practice's financial health. To address these problems, healthcare providers must focus on the importance of accurate billing and coding when selecting billing services.
Simple data entry mistakes, such as transposed numbers or incomplete patient information, often cause common errors. Incorrect coding can wrongly process claims, resulting in significant financial loss in practice revenue.
Miscommunication with insurance companies and payer relations frequently costs practices time and money.
To address these problems, providers must follow best practices in billing audits, such as keeping detailed billing records and routinely reviewing claims carefully.
By ensuring the billing team maintains accuracy and care, practices smooth the billing process, leading to quicker payments and improved revenue.
6. Difficulty with Communication
Difficulty with communication between healthcare providers and billing companies can lead to misunderstandings, adversely impacting the efficiency of billing services and claims processing software and compliance with industry regulations. Setting up good customer relationship practices keeps communication open and allows quick follow-up on claims.
To improve this important conversation, organized communication methods, such as regular updates, telemedicine billing, and planned meetings between billing professionals and healthcare teams, are necessary.
Such proactive engagement fosters a collaborative environment and healthcare industry engagement, allowing teams to address and resolve issues promptly, reducing the likelihood of costly errors or delays.
Secure messaging platforms simplify communication and medical office solutions, ensuring everyone receives instant updates about the status of claims and compliance rules.
By prioritizing clear and consistent communication, billing companies and healthcare providers work together more effectively, ultimately improving service delivery and patient satisfaction.
7. Potential for Data Breaches
In healthcare finance, data breaches and billing errors pose a major threat to practices using medical billing services that lack strong data security and do not follow regulatory rules.
Businesses must work with billing companies that use modern billing technology to protect patient data and maintain connections between billing systems and medical billing software.
Without these important safeguards, practices risk losing money and damaging their reputation, leading to a loss of client trust.
Following rules like HIPAA constitutes a legal duty and represents an important part of providing ethical healthcare.
Investing in secure billing technology fortifies organizations' defenses against cyber threats while demonstrating their commitment to safeguarding private data.
This approach reduces risks of data breaches and improves the integrity of the billing process. This approach creates a trustworthy and secure setting for healthcare providers and patients, enhancing patient accounts management. For those evaluating cost-effective solutions, it's worth exploring: What's the Cheapest Medical Billing Service in 2024?
8. Limited Technology and Software
 Limited technology and software capabilities in billing companies hinder operational efficiency and reduce the effectiveness of billing automation processes, potentially affecting revenue cycle optimization for healthcare providers. Investing in advanced billing software and seamless software integration improves billing metrics and provides cost-effective solutions and overall service quality.
Limited technology and software capabilities in billing companies hinder operational efficiency and reduce the effectiveness of billing automation processes, potentially affecting revenue cycle optimization for healthcare providers. Investing in advanced billing software and seamless software integration improves billing metrics and provides cost-effective solutions and overall service quality.
Modern billing software simplifies processes and allows quick and accurate submission of claims.
Billing automation reduces human errors, improves billing workflows, and ensures smooth payment posting and patient invoicing.
Healthcare providers can use information gained from analytics to make data-driven decisions that improve their revenue processes.
Software integration plays an important role by linking different operational systems in revenue management services, smoothing workflows, reducing administrative work, and improving communication among those involved.
This complete method guarantees quick reimbursements and better service for providers and patients.
9. Lack of Compliance with Industry Standards
Non-compliance with industry standards in billing services leads to costly errors, increased claim denials, and potential legal issues for healthcare providers. Healthcare providers need to follow billing rules and handle denials well to keep the revenue cycle management process running smoothly.
Healthcare providers must stay informed about the latest billing regulations, as it is essential for safeguarding the financial health of their practice through effective billing analysis. Healthcare practices must regularly check for updates in laws and industry guidelines due to changing rules and standards in healthcare billing.
Regular training for staff and thorough checks help reduce the risk of breaking rules. By following a consistent approach for billing and managing practices, healthcare providers can reduce interruptions, improve cash flow, and raise patient satisfaction.
Following these practices shows careful attention and dedication to providing top-notch care for patients.
10. Potential for Legal Issues
Improper billing practices can lead to legal issues, underscoring the importance of strict compliance with billing regulations and ethical standards in healthcare finance. Healthcare providers must vigilantly select billing services to mitigate risks associated with insurance claims processing and maintain financial integrity.
Adhering to these regulations prevents severe legal ramifications, including hefty fines, sanctions, or even criminal charges for fraudulent billing activities. Patients and insurance companies might sue doctors and hospitals, complicating their financial issues.
To avoid these pitfalls, practices must implement thorough training programs for staff on ethical billing practices and regularly audit their billing procedures. Engaging reputable billing companies that prioritize compliance with current laws safeguards against inaccurate claims, ensures that billing processes align with industry standards, and protects the practice from potential legal repercussions.
What Is a Medical Billing Service and What Does It Do?
A medical billing service manages billing tasks for healthcare providers. This includes managing insurance claims and billing patients, which is important for managing the flow of money in healthcare. Medical billing services make these tasks easier, so providers can focus on giving quality care to their patients while making sure payments are processed quickly and correctly, helping to maximize revenue.
The different tasks these services perform, such as accurate coding, timely claims submission, and quick payment handling, are essential for maintaining a clinic's cash flow stability.
These services carefully check and code medical procedures to follow current rules, decreasing the chances of rejections. Looking over denied claims is important so that the healthcare organization gets all the money it is owed, which is necessary for keeping its finances stable.
These services improve practice operations and allow practices to dedicate more resources to patient care and achieve better treatment results.
What Are the Key Factors to Consider When Choosing a Medical Billing Service?
 When selecting a medical billing service, healthcare providers must consider several key factors, including billing compliance, client satisfaction metrics, and the range and affordability of offered billing services. This ensures alignment with their specific needs and helps to promote effective revenue cycle management.
When selecting a medical billing service, healthcare providers must consider several key factors, including billing compliance, client satisfaction metrics, and the range and affordability of offered billing services. This ensures alignment with their specific needs and helps to promote effective revenue cycle management.
Assessing the experience of the billing service provider gives healthcare providers an idea of how well they handle the complicated processes of insurance claims and reimbursements.
Customer support plays an important role because clear communication greatly affects how problems are solved and how happy customers are with the service.
Carefully reviewing pricing models ensures cost savings. Knowing the differences between fee-for-service and percentage-based models helps you make a good financial decision.
Careful research in these areas helps practices prevent problems and choose a partner that simplifies tasks and improves their financial condition.
What Are the Common Mistakes Businesses Make When Choosing a Cheap Medical Billing Service?
Businesses often make common mistakes when they opt for the cheapest medical billing service, such as overlooking the importance of coding accuracy and failing to review client feedback, which can lead to detrimental outcomes. Knowing the advantages and disadvantages of all-inclusive packages helps businesses make good decisions in managing medical offices.
Organizations often find that choosing a cheap option results in poor assistance, with very few resources available to handle questions or problems.
Poor compliance with industry regulations exposes a company to legal risks and financial penalties, underlining that the initial savings may not justify the long-term repercussions. Hidden fees often accompany these lower-priced services, further compounding an organization's costs.
To reduce these risks, businesses should focus on quality rather than just cost and carefully research to find a dependable partner that matches their operational needs.
Affordable Medical Billing Service Statistics
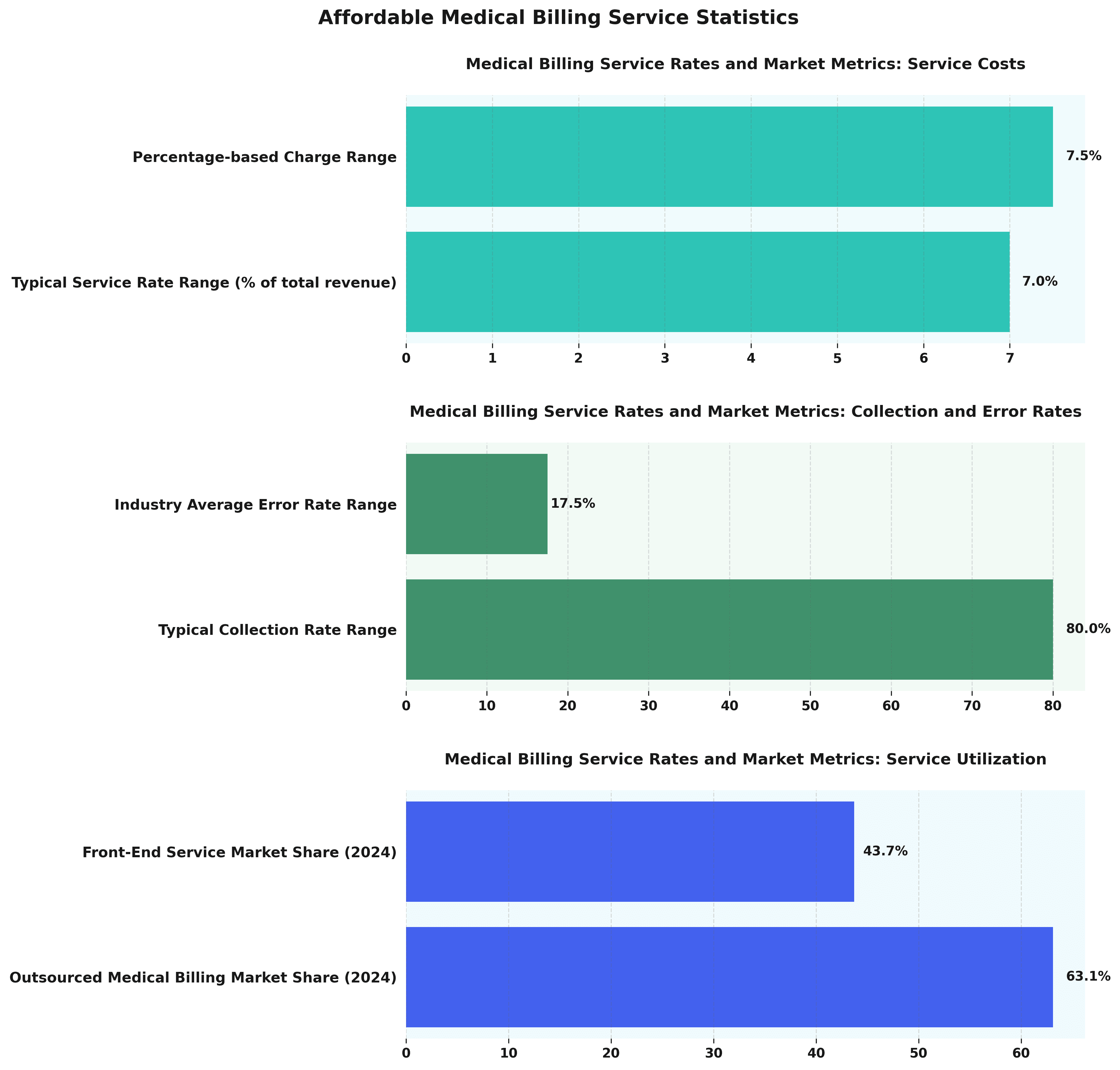
The Affordable Medical Billing Service Statistics provide information about expenses, efficiency, and use in the medical billing field, focusing on changes in telehealth billing. Grasping these metrics is important for healthcare providers who want to improve their revenue cycle management and make their operations run smoothly.
Medical Billing Service Rates and Market Metrics reveal key trends. Service costs are notably characterized by a typical service rate range of 7% of total revenue, coupled with a percentage-based charge range of 7.5%. This indicates that medical billing services often operate within a narrow margin, highlighting the importance of cost-effectiveness in outsourced solutions.
- Collection and Error Rates: Medical billing services demonstrate a typical collection rate range of 80%, underscoring the efficiency of these services in retrieving payments. However, an industry average error rate range of 17.5% suggests that there are significant opportunities for improvement, particularly in reducing billing errors which can impact collections and patient satisfaction.
- Service Utilization: The data reveals a 63.1% market share for outsourced medical billing In 2024, highlighting the increasing use of outside companies to handle billing tasks smoothly. Furthermore, a 43.7% market share in front-end service usage suggests a strong demand for services that handle tasks such as patient registration and insurance verification, which are critical for minimizing errors and streamlining the billing process.
The Affordable Medical Billing Service Statistics highlight the need to improve medical billing methods to manage both cost and efficiency effectively. With high outsourcing rates and significant market shares in front-end services, the industry continues to evolve, driven by the need to improve accuracy and collection rates. By focusing on reducing error rates and enhancing service delivery models, medical billing services can offer even greater value to healthcare providers.
How Can a Business Determine If a Cheap Medical Billing Service Is Right for Them?
To determine if a low-cost medical billing service meets their needs, healthcare providers should consider things like how accurate the financial reports are, what services are provided, and how it might affect their practice's profit, including expense reduction. Evaluating these elements will help providers make informed choices that align with their financial goals.
Beyond basic cost considerations, providers should also assess the quality of service, such as billing accuracy and turnaround time.
The accessibility and responsiveness of customer support can significantly influence day-to-day operations. Checking how these services work with current systems is also key to making sure changes go smoothly.
Providers should look ahead to how a low-cost billing solution may affect long-term revenue cycle management to anticipate any negative repercussions that could arise from compromised service quality over time.
What Are the Long-Term Effects of Choosing a Cheap Medical Billing Service?
Selecting a low-cost medical billing service can cause serious problems over time, such as ongoing mistakes in billing, more denied claims, and lower payments from healthcare providers, which might risk the financial security of a practice. The consequences of short-sighted decisions can echo throughout a practice's revenue cycle management.
While initial cost savings appeal, billing errors accumulate quickly, leading to time-consuming reworks and unnecessary delays in payment collections.
Medical practices often struggle to settle disagreements and correct errors, diverting resources from patient care to paperwork.
Frequent billing problems harm a practice's reputation, causing patients to avoid services and reducing both income and trust in the practice.
Choosing a cheaper option causes repeated problems in operations, worsening the issue and leading to higher financial costs later on.
How Can a Business Maintain Quality and Accuracy with an Affordable Medical Billing Service?
Businesses can keep quality and accurate results and save money on billing by doing the following: regularly tracking claims and managing insurance billing, following billing rules and keeping up with billing updates, and concentrating on accurate coding and efficient charge collection. Businesses can safeguard their financial management and revenue cycle solutions by closely monitoring performance metrics with healthcare technology and billing management and engaging in regular audits to improve healthcare administration.
Besides these practices, organizations should set up clear communication rules to support teamwork between billing staff and healthcare providers, such as doctors and small practice billing. By ensuring that lines of communication remain open, organizations can quickly address any discrepancies or questions that may arise, enhancing medical reimbursement.
Medical billing companies often learn important information from client feedback to know what changes will make the customer experience better.
Regular performance reviews highlight areas for improvement and recognize successes, reinforcing effective billing strategies. This helps build a habit of always getting better, which can greatly improve how administrative services are provided.